Predicting Survival in Repaired Tetralogy of Fallot: A Lesion-Specific and Personalized Approach.
Ghonim S, Gatzoulis MA, Ernst S, Li W, Moon JC, Smith GC, Heng EL, Keegan J, Ho SY, McCarthy KP, Shore DF, Uebing A, Kempny A, Alpendurada F, Diller GP, Dimopoulos K, Pennell DJ, Babu-Narayan SV.JACC Cardiovasc Imaging. 2022 Feb;15(2):257-268. doi: 10.1016/j.jcmg.2021.07.026. Epub 2021 Oct 13.PMID: 34656466
Take Home Points:
- No single risk factor adequately predicts mortality and ventricular arrhythmias in rTOF
- In patients with a repaired TOF, the following factors emerged as independent on multivariate analysis:
- RVLGE – HR 11.4 (95%CI 2.7-4.8, p=0.001) – first study to show this
- LVLGE
- RVEF <35%
- LVEF <35%
- BNP levels >127ng/L
- Peak VO2 <17ml/kg/min
- Sustained atrial arrhythmia
- Age 50 or greater
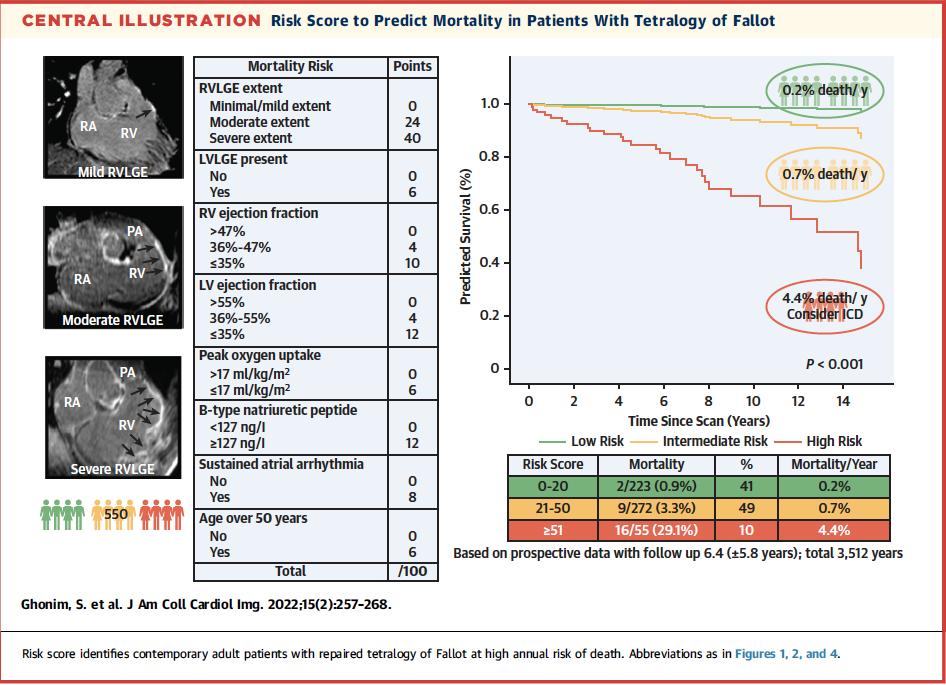
The weighted risk score described in this paper delineates the high-risk categories for mortality and for ventricular arrhythmias

Commentary from Dr. Blanche Cupido (Cape Town, South Africa), chief section editor of ACHD Journal Watch:
The growing population with repaired Tetralogy of Fallot (rTOF) frequently experience late consequences like premature death (including SCD), and ventricular arrhythmias. The evidence base to direct accurate risk stratification in this group remains inadequate. Observational studies have implicated a number of haemodynamic, electrophysiological and structural factors, though no single factor in isolation has been able to predict VT or SCD with certainty. The challenge remains balancing the risk of VT/SCD against the complications of inappropriate shocks with ICD implantation.
This prospective cohort aimed to assess the prognostic value of late gadolinium enhancement (LGE) on CMR (non-invasive assessment of VT substrate) and to devise a weighted-risk score for the assessment of SCD and VT using all the proven independent risk factors.
Consecutive patients with rTOF > age 16 were enrolled prospectively at a number of academic centers in London between 2002 and 2019 for CMR LGE testing in addition to standard care (clinical examination, ECG, BNP, echo, CPET). Holter monitoring was only done if clinically indicated. Patients with contra-indications to CMR and gadolinium were excluded. In addition to the usual CMR protocol, LGE imaging was obtained for LV and RV. Two experienced operators were blinded in their assessments.
The primary endpoints were all cause mortality. Secondary endpoints included Ventricular arrhythmias (VA) including SCD, resuscitated ventricular arrhythmias, and clinically sustained VT (either sustained >30s, or requiring cardioversion).
A total of 550 patients with CMR LGE were enrolled. Fifty-seven percent were male. The mean duration of follow-up was 6.4 years – a total of 3512 patient-years. RV LGE was seen at all the surgical sites in all patients. 98% seen in the RVOT and 100% at VSD patch sites. LGE was also found in RV trabeculations and the RV moderator band in ±32% of patients. Non-apical LV LGE only seen in 7% (n=41 – infarct-related in 8, papillary muscle/trabeculations in 20 and rest related to VSD patch).
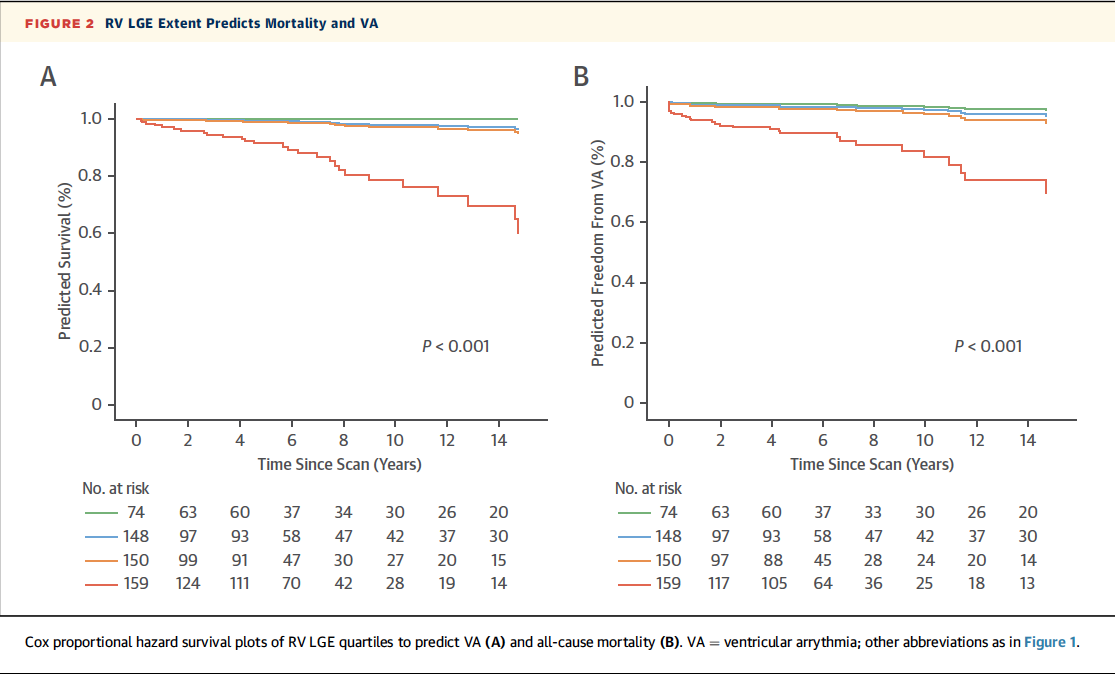
Twenty-seven deaths were recorded during the follow-up period – 13 SCD, 12 due to heart failure, 2 non-cardiac deaths. In addition to a number of univariate analysis factors, in keeping with past observational studies, RVLGE score of 5 or greater emerged as a predictor for higher mortality and ventricular arrhythmias. Figure 2 (above) illustrates that RVLGE predicted both mortality and ventricular arrhythmias.
Of note, Non-sustained VT (NSVT), previous palliative shunt, ventriculotomy, QRS duration >180ms and RV restrictive physiology were not univariate predictors of mortality.
On multivariate analysis, the following remained independent predictors of mortality:
- RVLGE – HR 11.4 (95%CI 2.7-4.8, p=0.001)
- LVLGE
- RVEF <35%
- LVEF <35%
- BNP levels >127ng/L
- Peak VO2 <17ml/kg/min
- Sustained atrial arrhythmia
- Age 50 or greater
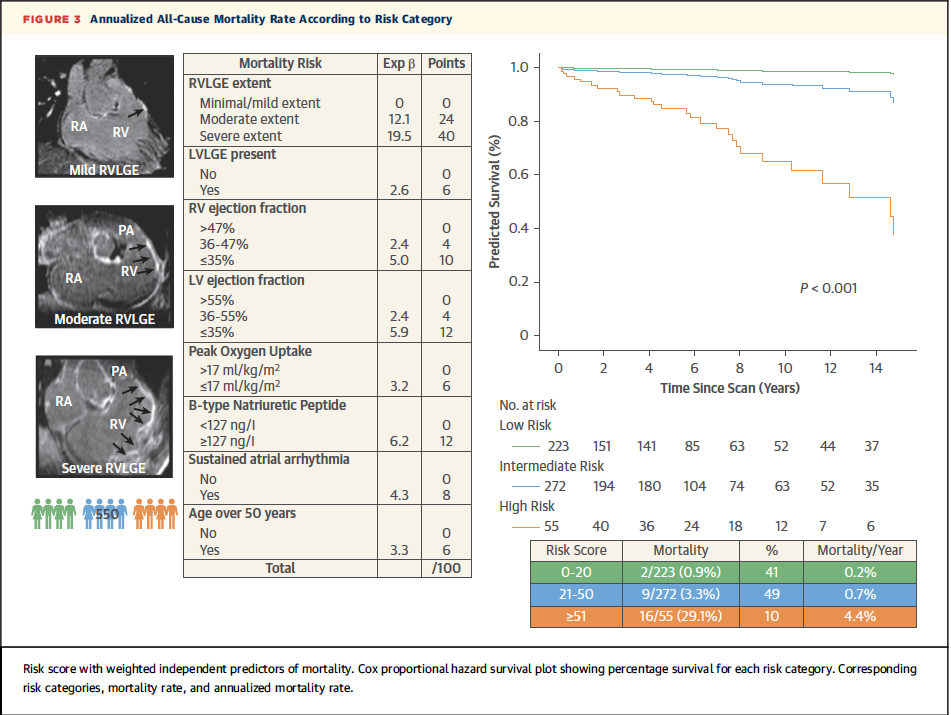
These factors were weighted and included in the development of the risk score depicted in Figure 3 above. A risk score of >51 had a 93% specificity and 51% sensitivity for mortality at one year. The high risk group portended a mortality rate of 4.4% per year. For every one point increase in the risk-score, there was an associated increase 7% risk of death (HR 1.07). Compared to a number of other existing risk models, this one performed better overall (AUC 0.87, 95% CI 0.78-0.95, p<0.001).
In terms of secondary outcomes – Ventricular Arrhythmias:
Twenty-nine patients reached the ventricular arrhythmia composite endpoint. RVLGE (fig 2 above) was predictive of ventricular arrhythmias. Other independent risk factors included: Restrictive RV physiology but only when associated with RV dilatation.

Similarly, the independent risk factors were devised into a risk score. For ventricular arrhythmias, a value of >40 demarcated the high-risk category with an annual rate of 3.7% events per year.

